The Norwegian National Advisory Unit on Tick-borne Diseases operates from Sørlandet Hospital in southern Norway. Our primary objective is to disseminate up to date knowledge about the etiology, diagnosis, treatment and prevention of tick-borne diseases, benefiting healthcare services, patients, and the general population in Norway. We are not a treatment center, but offer expert guidance and information to healthcare professionals, the public, and media outlets. Additionally, we conduct various educational workshops and lectures on tick-related topics. Furthermore, we actively initiate, support, coordinate, and participate in research projects and scientific networks. Funding for our endeavors is provided by the Ministry of Health and Care Services and Sørlandet Hospital.
For general questions regarding ticks or tick-borne diseases, please feel free to contact us via email at flatt@sshf.no. If you have questions related to your own health or containing other sensitive information, please use this link. It is secured for privacy purposes. Alternatively, you can reach us by phone at (0047) 38073329, Monday to Friday, between 10 am and 2 pm.
What are ticks?
Ticks are blood-sucking parasites that target birds, reptiles, and mammals, including humans. As arthropods, they belong to the same family as mites and spiders. With over 900 species globally, ticks inhabit diverse environments, spanning from temperate and tropical regions to the Arctic and deserts.

Ticks in Norway
About 9 different tick species are established in the Norwegian fauna. The sheep tick (Ixodes ricinus) is the most common species. The sheep tick is adapted for a temperate climate and is common throughout Europe. Like most ticks, the sheep tick is very small in size, usually between 1mm to 1,5 cm (when fully engorged). They feed off a variety of mammals and birds and can be found in woodland, grassy areas, gardens, parks etc. In Norway, they are particularly prevalent along the coastal stretch from Oslo to Helgelandskysten (close to Brønnøysund). Some areas have a high abundance of ticks, while some areas have none. Ticks don’t fly or jump but they crawl up grass or twigs for example and then latch on to animals or humans passing by. Once attached, they seek exposed skin to bite and feed. While a tick bite is usually benign, the diverse range of hosts they feed on, including rodents, birds, deer, and pets, exposes humans and animals to potential diseases known as tick-borne diseases.
Tick-borne diseases in Norway
In Norway, there are eight different diseases that can be contracted by humans through tick bites, with borreliosis and Tick-borne encephalitis (TBE) being the most prevalent. In highly endemic regions, such as coastal areas in southern Norway, approximately 25% of ticks carry the Borrelia bacteria, whereas less than 1% harbor the TBE virus. Additionally, various other microbes, including anaplasma, neoehrlichia, babesia, rickettsia, tularemia, and borrelia myamotoi, have been identified in sheep ticks in Norway, although only a few human cases have been reported. Despite the potential for disease transmission, studies have shown that the actual risk of illness following a tick bite is remarkably low, estimated at around 2%. Nonetheless, the incidence of tick-borne diseases has increased in Norway and several other European countries.
What should i do if i get a tick bite?
- If you get a tick bite, don’t panic. It’s a common occurrence, especially in Southern Norway. However, it’s important to remove the tick as quickly as possible. If the tick is removed within 24 hours, the likelihood of contracting borreliosis is very low.
- It’s important to note that the situation differs slightly for TBE, as this virus can be transmitted shortly after a tick bite. Removing the tick quickly doesn’t prevent TBE, but there’s an effective vaccine available for prevention.
- To remove a tick use a pair of tweezers, a tick removal tool or your own nails. Grasp the tick as close to the skin as possible and pull it straight out. Don’t be alarmed if the tick’s mouthparts remain in the skin (seen as a black spot). This does not increase the risk of tick-borne diseases.
- Some people lubricate the tick with butter, petroleum jelly or alcohol in an attempt to remove the tick. We do not recommend this, as it may delay tick removal.
- Contact a doctor if you experience any symptoms that can be related to the tick bite (see description of symptoms below).
What is borreliosis?
Borreliosis, also called Lyme disease, is the most common tick-borne disease in Norway and Europe. The disease is caused by a group of bacteria called Borrelia bacteria, which can be transmitted to both animals and humans through tick bites. Borrelia is widespread in the Northern Hemisphere. You can therefore become infected both in Norway and abroad. There are more than 30 different genospecies of Borrelia bacteria, but only some of the species cause disease in humans. In Europe and Asia, Borrelia afzelii and Borrelia garinii are the most common genospecies, but there are also other species that can cause disease (for example Borrelia burgdorferi sensu stricto, Borrelia spielmanii, and Borrelia bavariensis).
In 2023, there were 568 reported cases of systemic borreliosis in Norway (neuroborreliosis, borrelia arthritis, ACA, borrelia carditis etc). In addition, at least 7000 Norwegians are diagnosed with Erytema migrans every year. Erythema migrans is a skin infection (red rash) caused by the borrelia bacteria. Erythema migrans is the most common form of borreliosis in Norway/Europe (accounts for 95% of all borreliosis cases).
Symptoms of borreliosis
Borrelia usually only causes a skin rash, but can also give infektion the nervous system, joints and, rarely, the heart. See a doctor if you get symptoms of borreliosis after a tick bite. Borreliosis should be treated with antibiotics.
Erythema migrans
This red rash is the most common and often the only symptom of Lyme disease. This is a mild skin infection. The rash grows at the site of the tick bite, is larger than 5 cm, and occurs approximately 3-30 days after the tick bite. The shape, size, and color of the rash vary greatly. Additional symptoms such as malaise, headache, and muscle and joint pain may occur. At least 7,000 Norwegians get EM every year.
Borrelia lymphocytoma
Red/purple swelling in the skin (0.5 – 3 cm) that usually occurs on the earlobe, tip of the ear or nipple. This is a mild skin infection. Occurs days to months after a tick bite. Often near the tick bite. It is rare but more common in children.
Neuroborreliosis
Borreliainfection in the nervous system. Symptoms can vary depending on which nerves or brain membranes are affected. Symptoms typically occur weeks to a few months after a tick bite. The most common is facial nerve paralysis, the next most common is nerve inflammation causing significant pain in the neck/back, with radiating pain in the arms, legs, or as a belt from the back to the abdomen. Changes in sensation in the skin in the painful areas are common. Other paralysis and difficulties with coordination may also occur. Other common symptoms are headache, light sensitivity, neck stiffness, lethargy and feeling sick.
Borrelia arthritis
Borreliainfection in the joints. Inflammation in one knee joint is most common. One can also get inflammation in other large joints. The inflamed joint will often become very swollen and warm. It is not unusual for the swelling/pain to come and go in periods.
Acrodermatitis Chronica Atrophicans (ACA)
Red/purple/bluish inflammation of the skin that persists for many months/years. Most common in elderly women. ACA can damage the subcutaneous tissue causing the skin to become paper-thin and look old. Simultaneous muscle, joint and nerve pain (polyneuropathy) is also common.
Borrelia carditis
Borreliainfection in the heart. Can cause varying degrees of cardiac arrhythmias
How is borreliosis diagnosed and treated?
- If you develop a red rash (Erytema migrans) around the tick bite, that is larger than 5 cm, it’s important to schedule an appointment with a general practitioner. Blood tests are not required.
- If neuroborreliosis is supected it is necessary to be referred to a hospital for further evaluation. Both a blood test and a lumbar puncture should be taken and tested for Borrelia specific antibodies (antibody test).
- If borrelia arthritis is suspected, referral to a rheumatologist is recommended. A blood test (antibody test) is necessary. Additionally, a sample of synovial fluid should be taken and tested using a DNA test (PCR).
- If ACA is suspected, a blood test (antibody test) is necessary. Patients with ACA typically have high antibody levels. A general practitioner or dermatologist can also take a skin biopsy of the rash, which is tested for Borrelia DNA using PCR (polymerase chain reaction).
- All symptoms of borreliosis can be effectively treated with antibiotics. Erytema migrans is usually treated with Penicillin. Neuroborreliosis, borrelia arthritis, ACA etc is usually treated with Doxycyclin.
What is TBE?
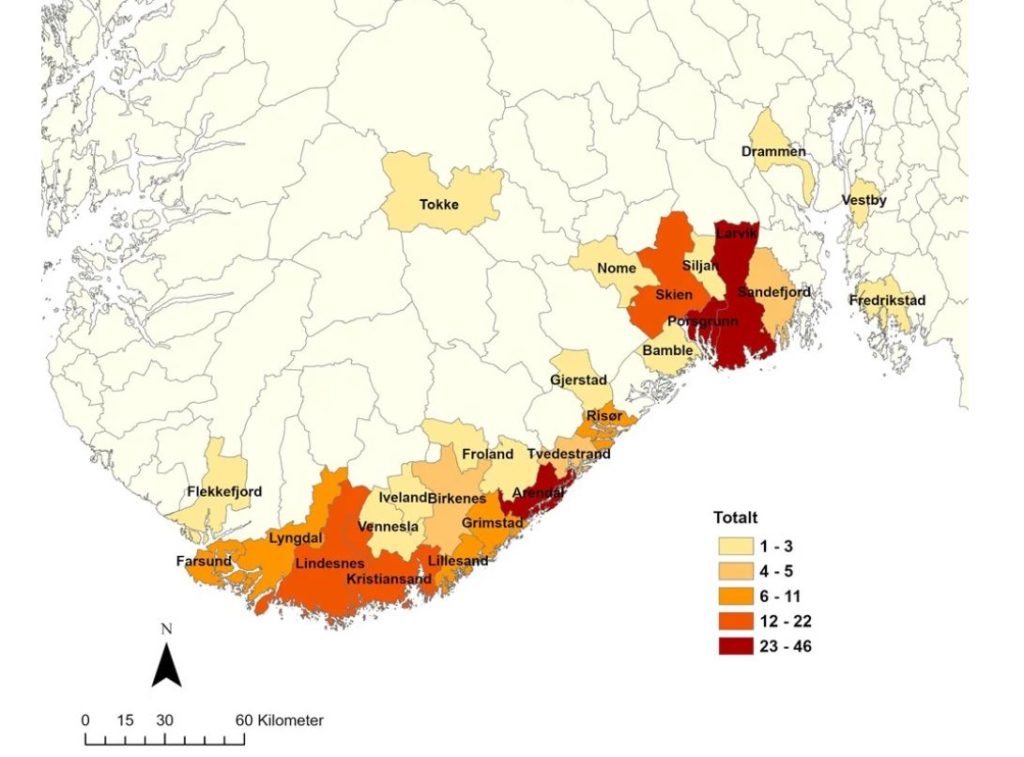
Tick-borne encephalitis (TBE) is caused by the TBE virus, a flavivirus. Subtypes include European, Siberian, and Far Eastern. In Norway, only the European subtype is present, transmitted by the sheep tick. The Siberian and Far Eastern subtype is mainly found in Eastern Europe to China and Japan. In rare cases abroad, consumption of unpasteurized milk or cheese from cows, goats and sheep can lead to infection. Symptoms vary greatly, from none to severe illness. Unlike borreliosis, where risk decreases if a tick is removed within 24 hours, TBE transmission can occur shortly after a bite. TBE incidence in Norwegian ticks is generally low but increasing. Less than 1% of ticks carry the virus on average, but local «hot spots» exist. In 2022, 84 people in Norway were diagnosed with TBE, with a majority requiring hospitalization. To date, human TBE cases have only been reported in the following counties: Agder, Telemark, Vestfold, Akershus and Østfold (see figure below). Coastal areas in these counties are the risk areas for TBE in Norway.
Symptoms of TBE
The incubation period for TBE ranges from 2 to 28 days. While some individuals may experience no symptoms (asymptomatic infection) or only mild symptoms, others may become very ill. A biphasic course of the disease is common, but not universal. The initial phase typically lasts about a week and resembles a «summer flu,» with symptoms such as moderate fever, headaches, muscle aches, and nausea/diarrhea. Some individuals may recover completely after this phase without realizing they were infected with the TBE virus, unless tested for TBE. However, others may experience a relapse with more severe symptoms (phase 2), including high fever, severe headache, lethargy, confusion, vomiting/diarrhea, neck stiffness, muscle aches, and paralysis. These symptoms indicate meningitis, encephalitis, and/or spinal cord inflammation. Adults, particularly the elderly, often experience a more severe illness compared to children. Hospitalization is common. The mortality rate for European TBE is less than 1%, while the Siberian and Far-Eastern types have higher mortality rates (up to 35%). In Norway, the first death due to TBE was recorded in 2022.
How is TBE diagnosed and treated?
The diagnosis of TBE is confirmed by detecting antibodies in blood and cerebrospinal fluid, along with inflammatory cells in the cerebrospinal fluid. In the early phase after infection, antibodies may not always be present in the blood, but TBE virus DNA can be detected early on with a PCR test. Approximately a week after infection, TBE antibodies (IgM and IgG) are formed. At this point, the PCR test is no longer positive because the viremic phase (the period when the virus is present in large quantities in the blood and tissues) has ended.
